Head and spinal cord injuries have existed since the dawn of time. In fact “neurosurgery” is thought to be the oldest medical specialty of all time.
Philosophers and physicians for thousands of years have tried to understand how the brain works. In 335 BC, Aristotle thought the brain was like a radiator that kept the heart from overheating. The ancient Romans believed the brain was the seat of complex thought and determined everything from bodily functions to personality.
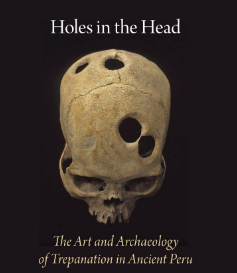 In ancient India, China, and Peru surgeons commonly removed portions of a patient’s skull to treat head wounds. The procedure was usually done after a battle and a similar procedure is done today to relieve the pressure caused by head trauma. There were many legitimate medical practices that were inspired by letting out evil spirits.
In ancient India, China, and Peru surgeons commonly removed portions of a patient’s skull to treat head wounds. The procedure was usually done after a battle and a similar procedure is done today to relieve the pressure caused by head trauma. There were many legitimate medical practices that were inspired by letting out evil spirits.
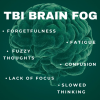
Despite astounding medical progress over the centuries and increased survival rate, traumatic brain injury survivors now have a different set of obstacles to overcome. Instead of life or death, patients and the medical community now have to face quality of life problems.
Continuum of care for TBI
The continuum of care for people with traumatic brain injury has become a lot more complex as medical technology continually increases survival rates. These increased survival rates equate to more patients living with severe deficits.
To ensure maximum recovery, the patient needs to be provided the opportunity in a setting that is conducive to the best recovery. And in this instance, Dorothy was right, there is really no place like home, especially for the brain-injured individual. Many patients have remarkable improvement with quality treatment, appropriate settings and sufficient time to be treated.
The acute hospital, subacute program, post-acute program, and home program should all be considered equal in the continuum of care. A best practice for everyone involved is that timely movement to the appropriate setting maximizes recovery.
The importance of home and community in brain injury rehabilitation

According to the CDC, there are 1.4 million Americans that sustain a brain injury each year. Brain injuries result from falling, car accidents, assaults, and other incidents in which the skull is penetrated by being forcefully struck.
Some people incur life-threatening injuries that need immediate hospitalization and extended rehabilitation. But most are seen in emergency rooms and discharged with little information about any impact that might change their life. Each brain injury is different.
Acute Hospitalization Phase
The immediate aftermath of severe brain injury can be very confusing. The patient is immersed in an intensive care unit where a “good” day of progress can be quickly followed by a “down” day of setbacks. Setbacks are common and don’t mean permanent reversal. If the patient stabilizes then will be transferred to a regular patient room in the hospital and go through early rehabilitation.
A neuropsychologist will usually do an assessment to evaluate what abilities the person with a brain injury has preserved. This evaluation helps the individual and the family understand how the injury has affected intellectual functioning. It also provides valuable information about how to treat the deficits. This will indicate the kinds of care the injured person will need.
The Rehabilitation Phase 
Following acute hospitalization and early rehabilitation, some people with brain injuries will go to specialized rehabilitation programs to continue the recovery process. Others who have significantly improved go to transitional live-in programs to fine-tune cognitive and vocational skills before returning to the community. But the goal is always to return home to normalcy and daily routines.
During this rehabilitation phase, medical issues are no longer the primary concern, and more emphasis is placed on cognition (the way a person interacts with their environment). The goal is to build skills and prepare. Whether that means going back to school, work, or the family home, the aim is to help them enjoy the highest quality of life possible. Unfortunately many return to the community without these follow-up services.
There’s no place like Home and Community
It’s very upsetting for the injured person to realize he or she has limitations, and as a result, behavioral problems occur. Being at home in a “real world” setting allows the clients to transition from the hospital or clinic to their own space. Involvement with family and the community improves functional outcomes.
According to a survey conducted by NeuroPraxis on patients who had completed the home and community re-integration program, 10 out of 10 reported that they had a vast improvement in these specific areas:
Attention and concentration
- Memory
- Anxiety
- Depression
- Fatigue
Care for Brain Injury Rehabilitation
Everyone with a brain injury wants to go home, but depending on their level of recovery, their needs can vary dramatically. Each patient is different because each situation and injury is different. But one thing is for sure the positive results are overwhelming if therapy takes place in a “real world” setting. Because this allows patients to integrate and generalize new skills that directly relate to particular needs.
How is this measured and achieved?
- Case Management
- Occupational Therapy
- Physical Therapy
- Speech Therapy
- Recreational Therapy
- Life Skills
In the NeuroPraxis series on the Continuum of Brain Injury Care, we will explore the levels of care that are available for post-acute brain injury patients and the goals and objectives for each. We will also go in-depth in the coming weeks about identifying the assessment tools that are useful in measuring progress and outcomes.
At NeuroPraxis, we always keep in mind that the goal is to get injured individuals home and thriving.