Acquired Brain Injury: A type of brain injury sustained through an event that occurs sometime after birth.
Activities of Daily Living (ADL): The routine, everyday self-care activities of personal hygiene such as bathing and dressing, as well as such activities as feeding and walking.
Acute Care: Specialized hospital care for patients requiring specific types of medical attention.
Acute Rehabilitation: Cognitive and physical rehabilitation that takes place in a medical facility, usually following stabilization after an injury event.
Adaptive Equipment: Any specialized assistive device that aids in performing mobility, exercise, self-care or work/leisure activities.
Agitation: An inability to relax or obtain rest due to varying internal or external factors.
Alternative/Augmentative Communication: Non-verbal types of communication, such as writing, typing, sign language, computer programs and picture boards used to facilitate communication when someone is unable to communicate through verbal means.
Ambulate: The ability to walk.
Amygdala: It processes fear and triggers anger.
Amnesia: A loss of memory of prior events from specific time periods that sometimes follows a head injury event.
Aneurysm: The occurrence of an abnormal bulge or ballooning inside the wall of a blood vessel, which can result in internal bleeding and death without treatment.
Anomia: Type of aphasia marked by a person being unable to recall the names of common, everyday objects.
Anosmia: A loss of the sense of smell, which may be full or partial.
Anoxia: The loss of oxygen supply to tissues, which results in the death of cells.
Anterograde Amnesia: A loss of the ability to form new memories after a traumatic brain injury. Making new memories can be difficult or impossible.
Anticonvulsant Medication: A class of medications used to control and/or reduce the occurrence of seizures.
Antidepressant Medication: A class of medications used to manage the symptoms of depression.
Anxiety: An excessive and persistent feeling of worry and fear about everyday situations
Aphasia: An acquired communication disorder impairing the ability to effectively process or express language.
Apraxia: A motor disorder caused by damage to the brain resulting in a person having difficulty with carrying out every day movements.
Assistive Equipment: Specialized types of tools that assist with making tasks easier for those with an injury or disability.
Ataxia: A lack of muscle control or coordination of voluntary movements, such as walking, reaching, lifting or picking up objects.
Atrophy: A condition causing the wasting away of body tissue and/or organs, often due to cell degeneration.
Attention: A person’s ability to focus on a specific task.
Balance: The ability to maintain a sense of equilibrium.
Bilateral: Relating to both the right and left side of a person’s body.
Brain Scan: An imaging of the brain obtained through specific types of x-rays.
Brain Stem: Area at the brain’s base that serves as an automatic control for body functions such as heartbeat, breathing, blood pressure, involuntary muscles, consciousness and swallowing.
Case Manager: A professional who carries out the access, delivery and coordination of healthcare and supportive services for someone with special healthcare needs.
Catheter: A flexible tube inserted into a body cavity that is used to withdraw excess fluids from the body.
Cerebellum: Portion of the brain located behind the upper part of the brain stem that coordinates movement and regulates muscle activity.
Chronic: A condition or illness that is of long duration.
Chronic Traumatic Encephalopathy (CTE): Brain injuries that are caused by repeated trauma to the head, resulting in degenerative brain disease.
Closed Head Injury: A type of head injury in which the skull and dura remain intact following the injury. The injuries can be minor to severe and life threatening.
Cognition: The mental process of acquiring knowledge and understanding through thought, experience and sensory cues.
Cognitive Flexibility: The ability to shift our thoughts or actions to respond to given situations.
Cognitive Rehabilitation: Specialized therapeutic treatments that address the cognitive problems that can occur following a brain injury.
Coma: A state of prolonged unconsciousness caused by disease or injury in which a person is unable to respond to external stimuli.
Communicative Disorder: A communication disorder impacting someone’s ability to comprehend, detect or apply language and speech to real-life interactions.
Computerized Tomography (CT): A combination of x-ray and computer images used to create pictures of your organs, bones and tissues for diagnostic purposes.
Concentration: The ability to maintain focus on a specific task.
Concrete Thinking: Reasoning that strongly focuses on observations of the physical world occurring around us.
Concussion: A type of traumatic brain injury (TBI) resulting from an injury to the head causing the head and brain to move rapidly back and forth.
Confabulation: A memory error in which someone presents inaccurate recollections without realizing they are doing so as a compensation for memory loss.
Confusion: A conscious state in which a person cannot self-orient and is unable to think clearly.
Contracture: A permanent tightening of the muscles, tendons, skin and nearby tissue that causes joints to shorten and become very stiff, making movement painful and difficult.
Contusion: A bruise or injury to the brain, resulting in bleeding and swelling inside the brain.
Convergence: Movement of the eyes inward to focus on objects that are moving closer.
Decision making: Decision making is the process of choosing between two or more courses of action.
Depressed Skull Fracture: A fracture resulting when broken pieces of the skull press into brain tissue.
Depression: A mental health disorder that negatively affects your feelings, thoughts, and behaviors.
Diffuse Axonal Injury: Brain injury resulting from head trauma in which the axons are sheared off or are damaged. The injury results in interrupted brain electrical transmissions.
Disinhibition: Inability to suppress impulsive behaviors and emotions, resulting in behavior that is not appropriate to the situation or setting.
Disorientation: A state of mental confusion in which someone might be unaware of their location, identity, the time, date or other information they would ordinarily know.
Distractibility: Inability to stay focused or to maintain attention.
Dura: The tough, outer fibrous membrane lining of the brain and spinal cord.
Dysarthria: A condition in which the muscles you use for speech are damaged or weakened or you have difficulty in controlling them, resulting in difficult or unclear articulation.
Dysphagia: A condition in which someone has difficulty or discomfort in swallowing food or liquid.
Edema: Swelling caused by an accumulation of excess watery fluid in body tissues or cavities.
Electroencephalogram (EEG): A test or record that detects electrical activity in the brain through the use of electrodes.
Electromyography: A diagnostic procedure to test and record the electrical activity and health of muscles and the nerve cells that control them through the use of electrodes.
Emotional Lability: Rapid changes in emotionality and mood, such as laughing, crying and anger that is inappropriate to the current situation or setting.
Endotracheal Tube: A flexible plastic tube inserted into the mouth or nose that serves as an artificial airway to assist patients with breathing.
Epilepsy: A neurological disorder resulting from abnormal activities in the brain. Symptoms of epilepsy can include confusion, disorientation and seizures. Epilepsy can result from an inherited genetic condition, disease or head trauma.
Fluent Aphasia: A condition in which someone is able to say phrases that sound fluent, but when examined more closely, lack meaning.
Foley Catheter: A thin, sterile tube inserted into the urinary bladder for the drainage of urine.
Frontal Lobe: Lobes in the front of the brain concerned with higher level cognitive functioning, including behavior, learning, personality and voluntary movement.
Frustration Tolerance: The ability to maintain persistence in a task despite challenges or obstacles.
Gait Training: Specialized physical therapy designed to help someone in learning to walk following an injury.
GI Tube: Gastronomy tube surgically inserted into the stomach that allows for feeding, liquids and medications to be administered.
Glasgow Coma Scale (GCS): A clinical scale used to reliably measure a person’s level of consciousness following a brain injury, based on assessing eye movements, speech and body movement.
Global Aphasia: The most severe form of aphasia, caused by damage to the left side of the brain, impacting receptive and expressive language skills and auditory and visual comprehension.
Headache: A painful sensation in any part of your head.
Head Injury: An injury to the head, brain or scalp, which may have a temporary or more permanent impact.
Hematoma: A solid swelling of clotted blood in the brain tissue, outside of the brain, between the brain and its covering or around the surfaces of the brain, which can be life threatening.
Hemiparesis: A weakness or paralysis occurring on one side of the body.
Hydrocephalus: A condition characterized by excess fluid build-up in the head, which can sometimes cause brain damage.
Hyperacusis: A hypersensitivity to sound.
Hyperphagia: Excessive hunger.
Hypothalamus: A structure in our brain that is responsible for releasing and inhibiting hormones.
Hippocampus: Critical for episodic memory, which is the ability to recall and mentally re-experience specific events from our past.
Hypoxia: A deficiency of oxygen in the blood, which can result in shortness of breath, confusion, increased heart rate and a lack of oxygen getting to tissue.
Immediate Memory: Often termed short-term memory, the capacity to store a small amount of information in memory and have it available for retrieval for a short period of time
Immediate Seizure: A seizure that occurs within 24 hours of a traumatic brain injury, resulting from abnormal brain activity.
Impulse Control: The ability to control one’s emotions and behaviors through their own volition.
Impulsiveness: Acting on impulse or without forethought to the possible consequences of such actions.
Incontinent: The inability to control bowel and/or bladder functions.
Independent Living: Community-based settings for individuals established to maximize their independence and personal choice.
Initiation: The ability to begin an activity or task independently.
Inpatient: Receiving medical services in a specialized setting outside of the home in which the person stays in a hospital or other type of medical facility.
Instrumental Activities of Daily Living (IADL): Daily living tasks of budgeting, schedule management, grocery shopping, meal preparation, housework and leisure activities.
Interdisciplinary Approach: Two or more specialists working in tandem to facilitate medical treatment, such as a physician, case manager and speech therapist collaborating on care.
Intracerebral Hematoma: Bleeding within the brain resulting from damage to a major blood vessel, through a rupture of the vessel within the brain or trauma.
Intracranial Pressure: Pressure caused by fluid build-up, such as cerebrospinal fluid accumulating inside the skull.
Judgment: The ability to understand and to be aware of the safety levels and possible consequences of different situations and then make good decisions with this understanding and awareness.
Kinesthesia: The awareness of body movement and position via sensory means.
Lability: State of having quick, volatile shifts in mood that are not appropriate to the situation.
Long Term Memory: Memory that involves the storage of information for an extended period of time.
Magnetic Resonance Imaging (MRI): Non-invasive medical imaging technology that produces, detailed, three-dimensional anatomical images of the body.
Memory: The ability to recall, retain and learn new information.
Mild Brain Injury: A trauma-induced disruption of brain function marked by loss of consciousness, loss of memory of events before or during the trauma or an altered mental or emotional state at the time of injury. Patient must not experience post-traumatic amnesia for more than 24 hours. Loss of consciousness, if occurring, must not be longer than 30 minutes.
Motor Control: Regulation of purposeful, voluntary movement via the nervous system.
Muscle Tone: The resistance of a muscle in response to being stretched.
Nasogastric Tube: A narrow, soft rubber or plastic tube passing through the nose and throat to the stomach, allowing for feeding or removal of stomach acids.
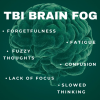
Neurofatigue: When your brain overworks itself and becomes “tired” due to a disruption in the brain’s circuitry system.
Neurologist: A physician specializing in the diagnosis and treatment of disorders of the brain and nervous system.
Neuron: A specialized, electrically excitable cell that transmits nerve impulses.
Neuropsychologist: A psychologist specializing in the relationship between the brain and how behaviors are related to the brain and nervous system. Often performs specialized testing to determine current brain and nervous system functioning.
Non-Ambulatory: Unable to walk or walk without the assistance of others.
Non-Fluent Aphasia: A condition in which someone has reduced speech, difficulty in recalling words and speaking in complete, understandable sentences.
Nurse Case Manager: A nurse who coordinates the medical care for an individual with complex medical needs.
Nystagmus: An involuntary repetitive, rhythmic side-to-side, up and down or circular motion of the eyes that occurs with a variety of conditions, often resulting in reduced vision.
Occipital Lobe: Area in the back of the brain that participates in visual processing. The occipital lobe is responsible for interpreting information from the eyes into how the person sees their environment.
Occupational Therapy: The use of assessment, treatments and interventions to help a person develop, recover and maintain the meaningful activities or occupations they previously engaged in.
Organization: The ability to methodically arrange your thoughts that enables you to communicate effectively.
Orientation: A sense of what is going on around you, such as knowing the date, time and year. Also, the sense of being able to familiarize yourself with your current environment.
Orthopedics: Medical discipline dealing with the treatment and correction of deformities or injuries to bones and muscle.
Outpatient: The receipt of medical services occurring when a person is not under in-patient hospital care.
Paraplegia: Paralysis of the legs, from the waist down, usually caused by injury or disease.
Parietal Lobes: Paired lobes at the top of the brain responsible for the reception and correlation of sensory information.
Penetrating Head Injury: A brain injury in which an object pierces the skull and enters the brain tissue, resulting in an open wound.
Perception: The ability to make sense of what one sees, hears, feels, tastes, smells or senses in their environment.
Perseveration: A response in which a person consistently persists in a task, action, behavior or thought that is not appropriate to the current circumstances or environment.
Persistent Vegetative State: An ongoing state of severely impaired consciousness in a patient in which they are unable to follow commands or make any meaningful response.
Physiatrist: A physician who specializes in physical medicine and rehabilitation.
Physical Therapy: The use of assessment, treatments and interventions to help injured or ill people improve their movement and manage pain.
Plasticity: The ability of the brain to adapt and organize itself in response to injuries and deficits.
Plateau: A leveling off of progress in recovery, which may or may not be permanent in nature.
Post-Acute Rehabilitation: Specialized programs providing intensive, 24-hour rehabilitation following an initial hospitalization designed to improve cognitive, physical, emotional and psychosocial skills.
Post-Concussion Syndrome: The persistence of concussion symptoms such as headaches and dizziness, for weeks and sometimes months after a concussive injury.
Post-Traumatic Amnesia: A state of confusion that occurs immediately following a traumatic brain injury, resulting in disorientation and the inability to remember at least some events that occurred before the injury.
Post-Traumatic Epilepsy: Recurrent seizures that occur more than one week following a traumatic brain injury.
Pre-Morbid Condition: Characteristics of someone’s physical, mental or emotional condition or level of functioning prior to the occurrence of disease or injury.
Primary Care Physician: Healthcare providers who manage a wide variety of healthcare concerns, serving as the first stop for most medical care.
Problem-Solving Skills: The ability to use logic and reasoning to address concerns and come up with resolutions in regards to them.
Processing Speed: The amount of time it requires for an individual to take in information
Prognosis: The likelihood of a person’s recovery from a disease, condition or injury over a span of time.
Psychiatrist: A physician specializing in the diagnosis and treatment of mental illness.
Psychologist: A professional specializing in the treatment of mental, emotional and behavioral disorders.
Quadriplegia: A partial or complete paralysis of both the arms and legs, usually resulting from a spinal cord injury or a disease of the neck region.
Range of Motion: The measurement of the extent of movement of a specific joint or body part.
Recreational Therapy: Utilization of recreation by therapists to promote independent functioning and enhance the well-being of persons with illnesses or disabling conditions.
Rehabilitation: A comprehensive program designed to address physical, mental, cognitive, speech, emotional and social deficits following injury or illness.
Rehabilitation Facility: A specialized health care facility that coordinates and delivers on-site services to address physical, mental, cognitive, speech, emotional and social deficits.
Residential Services: Long-term, 24-hour health care services provided outside of the home setting.
Retrograde Amnesia: Inability to remember events that occurred before a head injury. The amnesia might be for a specific time period or a certain type of information.
Seizure: A sudden, uncontrolled electrical disturbance between cells in the brain which can result in changes in your behavior, movements, feelings, cognition, awareness or level of consciousness.
Self-Monitoring: Ability to evaluate and observe your behaviors from others and allows you to compare your behaviors and adapt.
Sensation: A physical feeling or perception when the sensory organs of the body are activated, such as touch, temperature, pressure and pain.
Sensorimotor: Of or relating to functioning in both sensory and motor pathways as related to bodily activity.
Sensory Integration: Two or more sensory processes that integrate in a way that enhance brain adaptability.
Sequencing: The combining of information in a particular order or the ability to determine the order in which they are combined.
Short Term Memory: The capacity to store a small amount of information in memory and have it available for retrieval for a short period of time.
Shunt: A medical device that removes excess fluid from the brain and redirects it to another part of the body for reabsorption.
Spasticity: A condition of abnormal muscle stiffening or tightening, preventing normal, fluid movement.
Speech Therapy: The use of assessment, treatments and interventions designed to help a person regain normal speech and proper communication.
Stroke: A medical emergency occurring when a blood vessel that carries oxygen and nutrients to your brain is reduced or interrupted, which can result in impairment in the senses, cognition or bodily function.
Stupor: A state of impaired or altered consciousness in which a patient is unresponsive, but they can be aroused by a strong stimulus.
Subacute: Specialized, comprehensive inpatient care which may follow a period of acute rehabilitation and is not necessarily hospital-based.
Subdural: Situated or occurring between the dura covering the brain and the spinal cord.
Subdural Hematoma: Condition in which blood collects between the layers of tissue that surround the brain and is usually associated with a traumatic brain injury.
Supervised Living: Home-like setting in which a person who is unable to live independently is provided individualized care, supervision and support in the community.
Supine: Lying on one’s back.
Supported Independent Living: Person living in a home of their choosing, primarily independently, but with appropriate supportive services in place.
Tactile Defensiveness: Hypersensitivity to touch.
Temporal Lobes: Lower lobe of the cortex that is related to auditory processing, sorting new information, coding of memory and distinguishing smells and sounds.
Thrombosis: The formation of a localized blood clot at an injury site.
Tracheostomy: A incision that is made through the trachea that provides a passage to assist with breathing when the normal route is impaired or obstructed.
Transient Ischemic Stroke (TIA): A brief, stroke-like episode that results in temporary stroke-like symptoms, but can also be the precursor to a more serious stroke.
Transitional Living: A non-medical, usually temporary, living situation that provides training for individuals to be able to transition to more independent living options.
Traumatic Brain Injury (TBI): A disruption in the normal function of the brain that is usually caused by a bump, blow or jolt to the head or a penetrating head injury. TBI’s are characterized by a period of altered consciousness (amnesia or coma) that may vary in length. The related disabling conditions can be orthopedic, visual, aural, neurologic, vestibular, perceptive/cognitive, sensory, mental or emotional in nature. The disabilities from a TBI may or may not be permanent. Symptoms may appear immediately or days or weeks after the initial injury event.
Vegetative State: A specific chronic neurologic condition in which a person has a functioning brain stem but no consciousness or cognitive function.
Ventriculostomy: A neurosurgical procedure that creates a hole within a cerebral ventricle for the drainage of fluids.
Verbal Apraxia: A severe speech disorder marked by the impairment of control of the proper sequencing of muscles used in speech, including the tongue, lips, jaw muscles and vocal cords, making speech difficult.
Vestibular System: Parts of the inner ear and brain responsible for processing information that involves the sense of balance.
Visual Tracking: Eye movement ability that occurs when the eyes focus on an object as it moves across the field of vision.
Vocational Evaluation: A comprehensive evaluation administered to assess a person’s work skills and their past, current and future employability and earning potential.
Vocational Rehabilitation Counselor: A vocational specialist who focuses on social and vocational issues as they relate to a debilitating medical condition.